Personal stories reveal how anxiety, depression, and intergenerational trauma affect people across the Valley.
With just 45 psychiatrists for 12.5 million residents, mental health services struggle to meet growing demand.
The mental health helpline receives nearly 150 distress calls daily, helping those unable to access in-person care.
The waiting room hums with low voices and shifting footsteps. Each person carrying an invisible burden. A young man twists the zipper of his backpack over and over. He’s glancing at the clock every few seconds. A woman near him taps her foot in rhythm with the fluorescent lights overhead. Low, careful conversations can be heard across the room. Whispers about which therapies have worked, which doctors helped whom, and who missed appointments.
Near the far wall, a retired school principal from Ganderbal leans forward. His elbows on his knees, chin resting in his hands. For eight years, he has been bringing his 40-year-old son here. The son slouches in the adjacent chair, gazing toward the trees outside. He’s married, with a child at home, but the world seems remote. The fields that once required his hands lie untended. His meals go uneaten unless someone reminds him.
Desperation threads through the principal’s voice. “Some days he doesn’t leave his bed at all,” he says. “Everything is there, but his mind doesn’t allow him to live.”
A shuffle of papers, a cough, a tap of a foot. Each breath in the waiting room stretches time, weighed down by years of unseen strain.

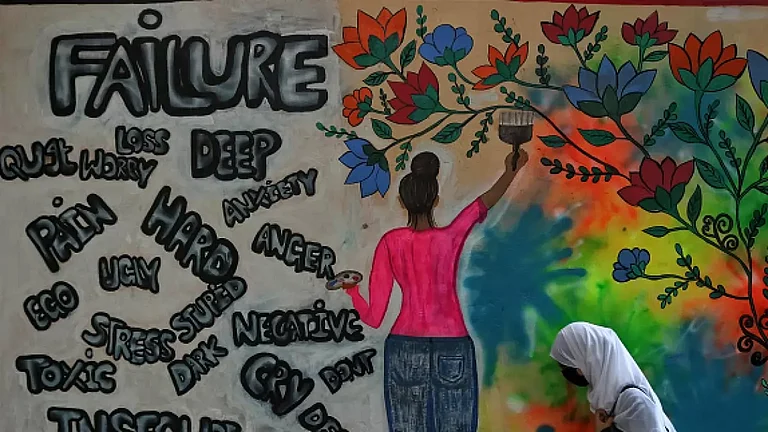
Between Walls And Hope
At the Hazratbal clinic in Srinagar, run by veteran psychiatrist Dr Mushtaq Margoob, known for decades of work on Kashmir’s mental health during the conflict, patients wait in clusters carrying histories that rarely fit into consultation slots.
The streets have largely quietened outside, but inside, the unease of the past lingers on.
“The trauma isn’t visible because no fighting is happening openly. People might feel well outwardly, as life seems calm, but that’s not how the brain or cognitive systems work. As a result of decades of unprocessed trauma, there is a silent burden that shapes daily life, even when the streets appear quiet,” says Dr Margoob.

A few seats away, a son keeps watch over his father, a man in his early 50s. The father’s hands rest on his thighs, shoulders trembling slightly with each exhale. “He used to move faster than anyone I know,” the son says, his voice edged with worry. “Now he just sits, waits, or stares. Nothing seems to reach him.”
Across the room, a young woman, barely twenty-two, perches on the edge of her chair, fingers interlaced in restless patterns. Her story spills out in fragments. Her parents’ separation, years of emotional neglect, long evenings spent staring at walls. She pauses often, searching for words. Her sadness spirals into tangents about sleep, food, and friends she has lost touch with. Her memory feels as frayed as the hem of her pashmina.
In her struggles, one can see the quiet weight of generational trauma, passed down through families in the Valley.
In one corner, Shamima, in her late 60s, presses her handbag to her lap, fingertips tracing its edges. She watches the room silently before she talks about her husband and son, who died years apart. After that, she began forgetting names and routines. When to cook, which plant needed watering, the small details that once anchored her day. As she talks, she folds and refolds her scarf.
These struggles are not isolated, as they reflect a broader mental health crisis gripping the Valley. According to the National Crime Records Bureau 2023 report, Jammu and Kashmir recorded 497 attempted suicides in 2022, the highest among all states and Union Territories. Of the 1,769 cases reported nationwide, more than a quarter came from the Valley.
Behind the front desk, staff shuffle papers and call out names softly, trying to impose order on a space that holds far more than appointments. The smell of antiseptic mingles with faint traces of incense drifting in from the nearby dargah.
The clock ticks stretching the wait that has become habitual for some and unbearable for others. Outside everyday life hums on. Vendors calling out, cars honking, children laughing.
At the Institute of Mental Health and Neurosciences (IMHANS), Srinagar, outpatient registrations have risen steadily over decades, from around 100 per week in 1980 to 850 by 2016. In 2024 alone, more than 2.03 lakh patients were examined in the outpatient department, with nearly 2,000 requiring admission.
According to the 2011 Census, the region has just 45 specialised psychiatrists for a population of 12.5 million. It is well below the World Health Organisation’s recommended minimum of three psychiatrists per 100,000 people.
Voices in Distress
While psychiatric institute sees patient loads, many are turning to helplines when in-person care is unreachable. A few kilometres away, across the Valley, another kind of waiting unfolds. Through Tele MANAS (Tele Mental Health Assistance and Networking Across States), the Centre-backed mental health helpline, people call from kitchens, living rooms, and offices and each conversation carries compressed hours of distress.
Dr Muhammad Abrar Guroo, Senior Consultant (Tele MANAS) at the Government Psychiatric Hospital, says the helpline receives nearly 150 distress calls a day in Jammu and Kashmir. This is the highest relative to population in the country. Of the 1,03,504 calls received so far, 87,450 were user-initiated, while 15,731 were follow-ups.
“These calls reflect stress, anxiety, panic attacks, adjustment issues, and academic or employment pressure,” Dr Guroo says. “What appears on paper as suicide numbers and hospital visits is only the visible edge of a much larger crisis. People reach out when the burden becomes unbearable.”
That morning, a 21-year-old student from Pulwama called as exams loomed, but panic attacks had forced him to abandon college for a year. His breathing raced, chest tight, heart hammering, until the Tele MANAS counsellor guided him through grounding exercises. By the end of the call, he leaned back against the wall, and exhaled. Tele MANAS, Dr Guroo notes, is an essential intervention when waiting becomes unbearable. Since video consultations were introduced in October 2023, more than 400 sessions have been conducted in the Union Territory.
“A phone call can help someone survive a moment,” he says. “But healing is a long process.”
Collective Trauma, Community Healing
Helplines can ease immediate distress, but communities that have lived through prolonged trauma respond differently to everything from personal crises and natural disasters, with distress often compounding rather than passing, says Dr Margoob.
Initiatives like Social Welfare and Awareness Bureau (Sawab), founded in the 1990s, take mental health care beyond hospital walls, working through engaging mosques, spiritual networks, and the community. These networks ensure patients are supported and reintegrated into daily life, especially in emergencies, such as avalanches or floods, where communities already burdened by years of conflict must cope with sudden loss and disruption.
In another part of Ganderbal, along chinar-lined roads, a man in his late 30s who has been under psychiatric treatment for over a decade spiralled after the death of his mother. Grief worsened his symptoms, leaving him withdrawn, vulnerable and unable to manage daily routines.
Community members with Dr Margoob working in coordination with clinicians stepped in to restore structure, arranged the funeral rites, and engaged the local imams and neighbours to ensure sustained support for the patient.
“People like him need care beyond prescriptions,” Dr. Margoob notes. “The brain remembers trauma even when the streets appear calm.”
Policy And Hope
Even as clinicians and helplines respond to urgent needs, systemic change remains slow as mental health infrastructure in Kashmir continues to lag far behind demand.
The proposed Jammu and Kashmir Reconciliation, Trauma Healing, and Dignity Bill, 2026, seeks to acknowledge decades of conflict, displacement, and psychological harm. It links trauma care and psychosocial rehabilitation to the constitutional right to life with dignity under Article 21. It states that since 2019, there has been an acknowledged decline in incidents of violence, creating an opportunity to consolidate peace through humane, preventive, and forward-looking measures. The Bill further states that the “unaddressed psychological trauma perpetuates cycles of fear, mistrust, anger, social fragmentation, and inter-generational harm.’’
End Of The Day
Back at the Hazratbal clinic, the Ganderbal patient who once wandered naked, and was tied in chains waits silently with a shawl draped over his lap. His eyes move slowly across the room. A steadiness that was absent years ago has returned, his father whispers to another patient. Nearby, the young woman traces the edge of her shawl. And Shamima murmurs aayats quietly.
By evening, patients leave clutching prescriptions, as if relief can be carried home in paper bags. Dr Margoob says, "Often patients arrive only after seeing multiple doctors for physical ailments, when years of untreated illness have taken their toll. By then, the effects are deeply entrenched, and recovery requires addressing the trauma itself, not just the symptoms. Stigma often delays care, leaving suffering hidden until it becomes severe.”
In that waiting room, hope endures quietly. A reminder that the past continues to shape the present.
This story is part of an ongoing series examining the long-term mental health impact of conflict in Kashmir.