Homeless individuals face chronic sleep deprivation, stress, and isolation, severely impacting their mental health.
Substance abuse becomes a coping mechanism for many, often leading to high-risk behaviors and worsening health conditions.
Despite NGO interventions, mental healthcare for the homeless remains largely neglected in policy and public discourse.
As the city’s bustle fades into the night, pavements transform into bedrooms for the forgotten. But beneath the open sky, sleep comes in fragments. Rajesh, a migrant from Katwal village in Haryana, rests underneath a flyover near Delhi’s Lajpat Nagar Metro station. Reflecting on his life on the streets, he says, 'Beghar toh koi hota nahi hai, sab kahi se ukhad ke hi sadak pe aate hain.' (No one is truly homeless; they are pushed into the streets after being uprooted).
Dibakar, who drags and places his mattress right next to Rajesh, overhears the conversation and interrupts: “Sleeping on the streets is not rest; it’s waiting―waiting for morning, for work.”
'Kabhi kabhi toh itna chidh hone lagta hai, gussa aane lagta hai. Samajh hi nahi aata kya ho raha hai,' he says. (Sometimes I feel so irritated and angry. I can’t comprehend what is happening).
He pulls a bidhi out of his pocket, lights it and asserts, ‘Ab sahab yeh sab ke baare mai toh tab soche na jab khaye khatir ho, aadhe waqt toh roti ki pareshani hoti hai’ (We can only think about all this if we have food to eat, half of the time it is difficult to even get food).
Beyond Survival: Maslow and Mental Health
American psychologist Abraham Maslow’s hierarchy of needs ascribes five sets of needs: physiological, safety, love, esteem and self-actualisation. These needs are arranged in a hierarchy of prepotency, meaning the basic physiological needs, those essential for survival, take precedence. The physiological needs include air, water, food, shelter, sleep and clothing.
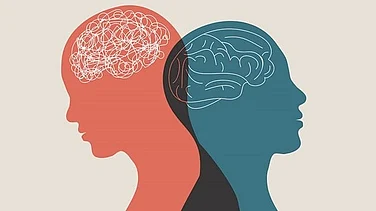
But can other issues prop up even if these basic needs aren’t met? Maslow noted that a need does not have to be fully met before a higher one starts shaping behaviour. Even for those at the lowest levels of society, higher needs can quietly influence their thoughts and actions, often without conscious awareness.
What then?
Kripanidh Kaur, a clinical psychologist practicing at the Institute of Psychiatry & Human Behaviour, Goa, highlights that since they are not getting any proper rest, their body is constantly in a fight or flight mode.
“Labourers perform physically demanding work throughout the day, engaging both mind and body. When sleep-deprived, their capacity to function at an optimal level diminishes. This disruption creates an imbalance, their muscles feel heavier, energy levels drop, and reflexes slow down. These impairments are a major factor contributing to on-site accidents,” she says.
Kaur adds that people in this demographic rarely report their mental health struggles. She explains how their issues transcend beyond rest or sleep. “A multitude of factors contribute to this issue. Many individuals face significant uncertainty and excessive stress in their daily lives. This increases anxiety. Migrating from their hometowns to urban areas often adds to their burden, leading to feelings of loneliness and isolation. All of these factors are deeply interconnected and compound one another,” she adds.
Coping with Crisis
For many like Rajesh and Dibakar, accessible stimulants like tobacco and alcohol help them stay awake and aid in relieving their perturbations. According to the 2011 Census data, India is estimated to house around 1.77 million homeless individuals. However, some non-governmental organisations estimate this number to be much higher.
During an unpublished 2021 pilot study by Ilam B.―conducted on a small sample of 100 homeless men in New Delhi―alcohol, cannabis, and opioid use were found to be significantly elevated: 76 per cent, 27 per cent, and 13 per cent respectively. While limited in scope, the study points to troubling trends in substance use within this vulnerable group.
In the World Drug Report 2020 published by the United Nations Office on Drugs and Crime, some countries have seen an increase in the use of illicit drugs over the course of the pandemic.
Sleeping under the Jamia Metro Station, Angad wakes with a start and takes a swig of Narangi, a cheap local liquor. Wiping his face with the back of his hand, he squints at the sunlight and asks, ‘Beedhi hai kya?’ (Do you have a beedhi?)
He glances around, slowly piecing together his surroundings. ‘Humara koi roz ka thikaana nahi hai. Sharab pee ke kya maloom kidhar sou. Humari biwi corona ke waqt marr gayi... ab kahin bhi sou, kya farak padta hai?’ (I don’t have a regular place to stay. After consuming liquor, I have no idea where I end up sleeping. My wife died during the COVID pandemic… now it doesn’t really matter where I sleep).
He pauses, and then mutters that getting through a day of work is easier after a proper night’s rest, something nearly impossible on the streets, unless numbed by alcohol.
Pushed Past the Margins
As one walks through the streets of Delhi or any major metropolitan city, stark instances of substance abuse and mental illness are often visible on the margins of society. How do these extreme conditions manifest? Case studies indicate that prolonged substance use or untreated mental health disorders, especially when compounded by chronic stress and uncertainty, can push individuals beyond the brink.
This high risk behaviour might not always restrict itself to mental issues. Trupti Desai, clinical psychologist and public health professional, shares the case study of a migrant worker from Rajasthan. She highlights how loneliness and fatigue led him to abuse substances like tobacco and alcohol. “As his substance use and engagement in high-risk behaviours continued, he also resorted to unsafe sexual practices as a way to cope with stress. Unfortunately, through these coping mechanisms, he contracted HIV,” she says.
Desai explains that since HIV often goes undetected without testing, his condition worsened over time. “It was only after several years, when he became severely ill, that he discovered he was living with the virus,” she adds.
“Often, when individuals are aware that something is wrong, instead of seeking help, they turn to substance abuse or risky behaviours. The fear of stigma and discrimination not only around HIV, but also mental health further deepens the crisis,” she says.
Sanjay Kumar, co-director of Aashray Adhikar Abhiyan (AAA), an organisation that works for the rights and mental health of the homeless since 2000, asserts that cases where labourers indulge in substance abuse due to multiple worries often leads to loss of livelihood. “This is the point where extreme deprivation pushes the homeless labourer over the edge. It’s when severe mental illness begins to take hold,” he says.
“According to our surveys, approximately 15 per cent of the total homeless population in Delhi has some form of extreme mental health condition. This data is only what is visible; there are countless more who are unaccounted for,” adds Kumar.
Is there Help?
Kumar says that a common characteristic among the homeless-mentally challenged individuals is that they only operate within a small radius. “There are a few hotspots that we have identified here in Delhi. For instance, we have zeroed in on Jama Masjid as it is a hub for these people,” he says.
He states that their organisation has some teams who go and observe possible cases in these flagged areas. “This makes it easier for us to track and give them treatment. We have partnered with psychiatrists from the Institute of Behaviour and Applied Sciences (IBHAS) and have set up rehabilitation camps where the team provides help to these individuals,” he says.
Dev Kumar, who supervises one of the mental health teams, says that addressing such cases was challenging under the Mental Health Act of 1987. “The Act included a clause that required court approval to assist a mentally challenged person found on the streets,” he says. “To overcome this limitation, we partnered with the Delhi Legal Services Authority and requested that a judge be present on the ground,” he added.
The Mental Healthcare Act, 2017, is better in this regard, he says. The new law lends the same power to a guardian who can vouch for the treatment of such individuals.
“We have also seen cases where substance abuse has proliferated among the homeless as they worry about their money getting stolen in the middle of the night or sometimes, or they fear that the police might take it. So, what they do is spend some money on food and buy alcohol from the rest,” says Kumar.
To address this, the Aashray Abhiyan has helped open bank accounts for the homeless. According to the latest data, Delhi currently has 66 permanent night shelters. However, many beneficiaries still sleep on the pavements, as rest in the shelters often comes in broken fragments. They continue to battle the harshness of the heat, which drives them back onto the streets.
Despite the continued efforts of NGOs and public health professionals to address this issue among the homeless, systemic and governmental safeguards remain largely inadequate. Mental health and related services are often burdened by the worries of stigma and lack of resources. As a result, mental health of the homeless remains absent in both policies and discussions.
Their struggles may fade into the hush of night, made invisible by indifference. And as people like you and me return safely to lie in warm beds, their heads rest on the same cold concrete beneath our passing steps―unseen, unheard and forgotten.