Britain is preparing for a Covid surge in late summer, with a planned, calibrated approach. Having practised under the National Health Service (NHS) for 30 years, Dr Ajay Vora brings an insider’s perspective to Britain’s ‘surge planning’. A paediatric haematologist with the Great Ormond Street Hospital, London, an institution with a storied past, he is in conversation with Sunil Menon:
An advisory has gone out to all medical establishments in Britain to prepare for a Covid surge in late summer. What’s the specific projection?
The modelling assumes an increase in infections as restrictions are lifted in a stepwise way, according to a roadmap that started in early April—children returning to school, all non-essential stores being open, restaurants and pubs being able to serve food and drink outdoors. From May 17, restaurants and pubs will be allowed to serve meals and drinks indoors, and people can meet in groups of six from three different households indoors. And then, from June 30, almost all restrictions will be lifted.
So this has nothing to do with any predictive model flowing from the virus’s life-cycle.…
No, it’s based on a combination of factors. Seeing infection rates fall, and a decrease in hospitalisation and deaths, due to a combination of vaccinations and the lockdown we had until early April. Over half the population has now received one dose and 10 per cent have received both doses. Data suggests that has reduced hospitalisations and deaths by 80 per cent. Those who get infected despite having been vaccinated have an 80-90 per cent lower risk of getting hospitalised. There’s also a reduction in transmissibility of 60-70 per cent after a dose of either the AstraZeneca or the Pfizer vaccines.
ALSO READ: The Missing Link Public Health
There are two critical terms in regard to how nations have responded to this outbreak. One is the elimination strategy, which China, New Zealand, Australia and Asian countries such as Korea and Japan have tried to follow, some more successfully than others. The second is a containment strategy…here, you accept that the virus will ultimately be endemic in your population, and your main aim is to reduce the number of people being hospitalised so it doesn’t overwhelm your healthcare system, as is happening in India, as happened in the US, and nearly so in the UK as well last December. And then prevent too many excess deaths, but accept that there will be excess hospitalisations and excess deaths from Covid. But you learn to live with that, as we have done with the flu virus. Every winter in the UK, we have 20- to 30,000 deaths from the flu virus. You expect that Covid might do the same.
The elimination strategy is predicated on having to go through recurrent localised lockdowns, like in Australia or New Zealand. Countries that don’t have as much international travel may be able to survive this way for years. But countries like the UK and the US can’t. We have accepted that we have to live with the virus, and adopt the containment strategy that does not impair the normal functioning of the economy and the healthcare system.
ALSO READ: We, The Makers Of This Calvary
The problem is, the virus, especially when it’s on this exponential phase of almost doubling every few days, is going to pick up new mutations. That’s the natural history of any virus as it spreads. And randomly, some of these mutations will give it a higher chance of transmissibility, which is what most of the mutants we have seen so far have acquired. And the fear is there will be a mutant that will allow the virus to escape vaccine-mediated immunity. So suddenly, we have not only the South African variant, in addition to the UK one, but also 100 cases of the Indian strains in the UK. But what we are not seeing is any indication yet that any of those strains are completely able to evade vaccine-mediated immunity.
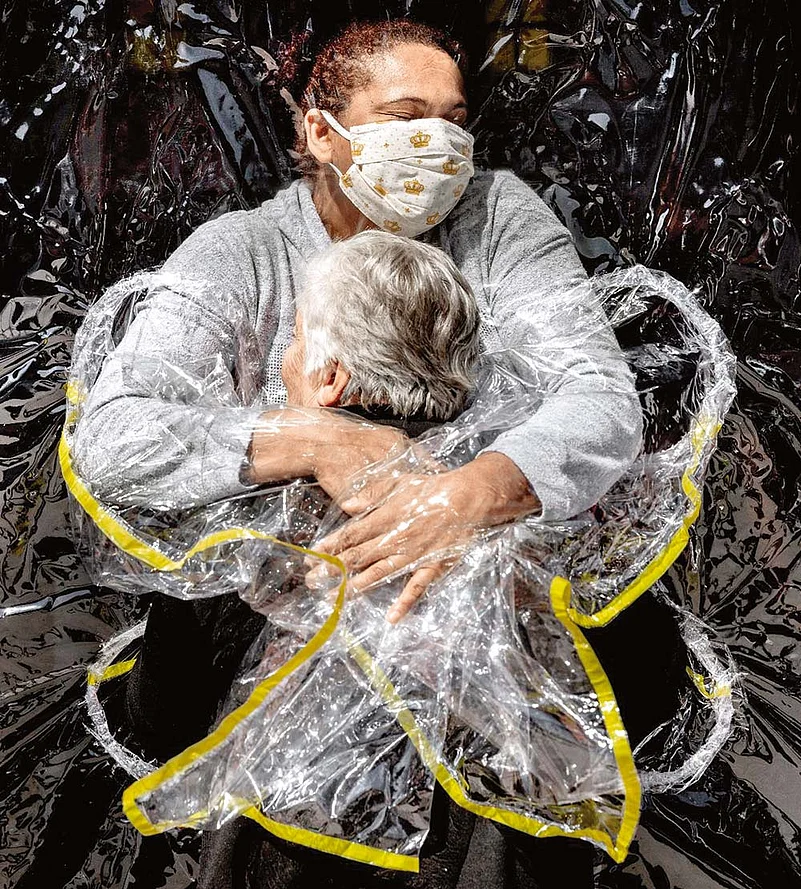
This photo symbolizing “love and compassion” of an 85-year-old Brazilian woman getting her first embrace in five months from a nurse through a transparent “hug curtain” is the World Press Photo of the Year.
What’s the exact nature of the preparations being made?
The roadmap anticipates that at every step, as we open up, there will be a rise in the rate of infections. But as long as it does not lead to an increase in hospitalisations and deaths, we don’t worry about it. Because as we go down the age-groups with our vaccination programme, we have now reached a point where almost 80-90 per cent of the most vulnerable are vaccinated with two doses. So the virus will circulate in the least vulnerable sections, where it will provide a degree of natural herd immunity. And eventually the vaccine programme will catch up with all adults above age 18 by the end of July. Both doses.
Yet, although 80 per cent of the vulnerable have received the vaccines, that still leaves you with a million or two among that vulnerable group who, for a variety of reasons, usually vaccine hesitancy, stay unvaccinated. So you are not going to contain the circulation of the virus to just within the young, less vulnerable group. And as we have discovered from India, even if 1 per cent of that young group ends up needing hospitalisation, that could overwhelm your system, because the absolute numbers are so great. So the intention is that you keep an eye on hospitalisations and deaths, not just on infection rates. If the infection rate climbs, so be it. If the other two are manageable, we continue on our roadmap of lifting restrictions. Obviously, there’s a risk that come June 30, when all restrictions are lifted, we have a situation like in Australia and New Zealand—where they are all walking around without masks—and there might be a sudden increase in the rate of infection. They have done some modelling on that. That could lead to a surge by August, which could require an expansion of healthcare capacity, which is where surge planning is happening. By designating certain hospitals that will shut down all their other activities, and just take Covid. And the other hospitals will soak up the non-Covid activity that that hospital was meant to do.
To what extent did non-Covid healthcare get affected in the UK last year?
There are two measures of that. One is the waiting list. The NHS, ever since it was set up in the 1950s-60s, has never been able to provide next day surgery or next week surgery for certain conditions. It’s always had waiting lists. For example, I had injured my knee. In India, with private insurance etc, I could have been operated on the next week. Here I had to wait six weeks for my operation on the NHS. Depending on which measure you use, the waiting lists run, on average, into about a million people waiting for some procedure or the other for between four and six weeks. Right now, there are 10 million people on the waiting list. So that’s one impact.
ALSO READ: Beating The Virus A Survival Guide
The second impact is more reassuring. That’s when you look at all-cause mortality. It’s one of the things we noticed in the UK and, I think, it has been seen elsewhere as well. My wife, for example, works in palliative care in a neighbouring hospital. What she noticed during the first wave was that most people dying of Covid were predicted to die of their underlying condition within three to six months anyway. Most of them had cancer or terminal heart or lung disease. They got Covid and died three to six months early. The term is anticipatory death. So when you look at six months hence, there are fewer people dying. Deaths from Covid plus other causes actually went to negative! We have rates, almost per week, over the last 20 years…how many people are expected to die, more people dying in winter, etc. During the first wave, there was a spike. As that receded, six months later, all-cause mortality went below average, as they had already died of Covid. Death had been anticipated. And then we saw a big spike from December to March because of Covid. Since March, we’ve gone into the negative again. Also, a lot of these conditions for which we have waiting lists are not what in NHS jargon we call P1, P2…which means you have to have your medical procedure within two weeks. That clinical prioritisation has remained intact. So those who needed whatever procedure within two weeks of being seen by healthcare professionals still got it. There were very few who did not….
The idea of surge planning seems to be rather conspicuous by its absence in India. With the salad bowl of mutations we might get with such a vast host population for the virus, there are scary predictions for July, November…. What do you think a country like India can do to forestall an even bigger wave?
Having practised here in the UK in a nationalised health service for 30 years, I would say the Indian government should just nationalise all healthcare, even if temporarily. Take over all private hospitals, and then use the command and control to say, for instance, ‘we’ll designate this big private hospital in Delhi as a Covid intensive care hospital, whereas AIIMS will do something else’. To some extent it has happened, with the government dictating to private hospitals that you have to reserve 80 per cent of your beds for Covid care. But I would really call for a temporary nationalisation of healthcare, maybe for two or three months. From a public health perspective, you also want a coordinated effort to ramp up all routine healthcare for people with non-Covid conditions—say, emergency cancer surgery and such like. That can only be done with a nationalised service. You can’t do it otherwise. This is why the US is struggling as well.
ALSO READ: Smother The Third wave
Would you call this the essential difference between the British and the Indian approach to healthcare?
Indeed, 95 per cent of our healthcare is nationalised. It’s the National Health Service. It’s got this command and control, with a lot of autonomy at the local level. Having that allows you to coordinate things more flexibly, rather than having private hospitals competing to grab slices of the most profitable pie. That’s the problem India and the US have—a bulk of tertiary care being provided by the private sector, which is only interested in what is most profitable.
As for the long term, that too requires a coordinated public health strategy. You have to have a strategy where you are doing a lot of genomic sequencing, so that you get an early indication of any worrisome mutant strains. Computer modelling—in silico modelling—tells you whether a particular mutant will be resistant to a drug, an immune mechanism or a type of vaccine. Then you go back to the laboratory and re-tweak the vaccine so that it will be effective against that viral strain.
We do that with the flu. The flu epidemic starts every year in the southern hemisphere, Australia, New Zealand, South Africa, during their winter. With the first signs of the flu, they sequence the strain. And design that year’s vaccine based on that. These are mutant strains: the backbone is still the same, but some of the Lego pieces have changed. You have to sequence the virus to find where those different Lego pieces are, then you design your vaccine. That’s the flu vaccine we then use in the West starting October—the flu eventually comes to us in the winter. Something like that will happen with Covid. Every year, we’ll have a new Covid vaccine. And that gets plugged into your overall public health strategy as well.
























